Read time: 12 minutes
Sujikka Suthakaran (Year 6) runs through how you can approach preparing for your summative OSCE assessment during your clinical years.
The thought of completing practical assessments at the end of the year can be very daunting, especially considering the large variety of skills and knowledge you will be tested on. However, the reason why OSCEs form part of our summative exams is to ensure that we become good and safe doctors by testing the important competencies that are required of one. It’s very normal to feel nervous about this exam but hopefully, by covering some of the different methods and resources you can use to prepare for your OSCEs in this article, this will alleviate some of the stress.
To prepare for your OSCE it’s important to understand the structure of the exam and the different types of skills that will be tested. There will be a Q&A session organised by the Assessment & Feedback Unit, so make sure you attend to find out more about this as well as the timings of the exam and what your role will be in the stations e.g. in Year 4 you will be a Year 4 medical student (although sometimes in a simulated FY1 setting) whereas in Year 5 (and Year 6) you act as a Foundation Year 1 doctor. All this information and more is available on the Assessment & Feedback Unit Moodle page.
There are several station types that you may encounter in your OSCE, however these are often integrated rather than a single type of station:
- Consultation skills
- Short clinical assessments
- Medical emergencies
- Practical skills
- Written communication & practical prescribing
With this in mind, here are some approaches you can take to prepare yourself for tackling these stations on the day of your exam.
Form an OSCE group
It can be difficult to know where to begin with preparing for the OSCEs, but the first thing you should do is to form OSCE groups, if you haven’t already. Whether it be your friends, flatmates or those in your firm, having a group of people you can meet up with on a weekly basis either in person or remotely to practise doing OSCE stations is really beneficial. You’ll get the opportunity to run through multiple stations from various resources testing lots of different skills. As such, this should help prepare you for how you approach each particular station when it comes to your OSCE.
A resource I would recommend is the book “OSCE Cases with Mark Schemes” which contains a variety of stations assessing different skills in each speciality in addition to detailed mark schemes. As you begin a new rotation, it’s often useful to start off by asking your OSCE group to practise history taking stations initially and then move on to explaining/interpreting stations to allow more time to go over the speciality topics thoroughly enough to answer the questions being asked in the station.
Check out the Moodle Assessment and Feedback Page
As mentioned before, the Moodle Assessment & Feedback Unit Page is the place to be for all things exam-related. It contains information regarding your exam dates, a summary of both formative and summative assessments, the methods by which your exams are marked in addition to sample OSCE stations which are in the OSCE resources section. I found the latter to be extremely helpful in understanding how certain topics can be assessed, how the mark schemes are structured and what information is important to mention in such clinical scenarios. It may be beneficial for you to attempt these stations closer to exams or after you’ve completed the speciality the station is linked to, as they can be slightly challenging and you may be better equipped to practise these stations after you have done some revision. Nevertheless, don’t let this stop you and you can even use these sample stations as a guide to create your own.
Not only are there practice stations within the OSCE resources, there’s a table with a summary of all the OSCE stations from 2013 onwards for your year group.
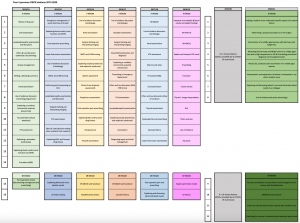
As the aim of these assessments are to test your competency of doing tasks required of a junior doctor, there are several skills that are tested each year which form part of the assessment criteria for your year group. For example, I’ve attached the previous Year 4 OSCE stations where you’re able to see the common skills that you are expected to know:
- History-taking and explaining management
- Examination skills
- Interpreting blood test results
- Performing procedures (ABG’s, cannulation)
- Knowledge about Ethics and Law
- Appropriately dealing with an emergency situation using a DRABCDE response (and being able to deliver a clear handover)
- Documentation in ward round notes and prescribing
- Communicating effectively with other healthcare professionals
- Knowledge about Use of Evidence
Therefore, practising these common skills whilst you’re on placement or with your OSCE groups will stand you in good stead when it comes to your exams. Again, you can use the previous station titles to come up with stations of your own or find similar stations online.
For fourth year students, you will have a dedicated Critical Care Day session during your Acute Medicine placement with the Clinical Skills team, where you learn to manage critically ill patients using a DRABCDE approach. Not only that, but you will also have the opportunity to practise mock OSCE stations, so use this session to clarify any doubts you may have and you can repeat these OSCE stations for revision closer to exams.
A Use of Evidence Station usually entails a patient coming in to see you about a research article they’ve read online; about a particular drug they’re taking or have heard about. You will be shown the abstract of the article and will be asked questions by the patient regarding what the conclusion of the article is, what certain words mean (e.g. sensitivity, number needed to treat) and whether you would recommend the patient taking the medication based on their history.
Considering that medicine here at UCLMS is a spiral course, you are expected to recall knowledge from earlier years in your later years. Therefore, based on this information you know that you will need to revise the statistics we learnt in CPP to do well in this station. This same principle applies to Ethics and Law stations as previously learnt knowledge is required in addition to attending your dedicated CPP sessions in fourth year. This tutorial is really useful in covering the important topics you need to know for both types of stations and is available on the Clinical years Treasure Trove (which contains lots of tutorials/resources to help you prepare for exams). I would also recommend creating Use of Evidence Stations yourselves, by finding research articles, looking at the abstracts and coming up with questions to ask so that you can practise doing these stations with those in your OSCE Group.
Spend time on the wards
Interacting with patients you meet is the best way to truly prepare for your exams, as you’ll be doing the same thing you did on the wards in an OSCE station under time pressure. Therefore, the more you speak to patients, the more prepared you’ll feel when it comes to exam day and thus, the better doctor you will be.
Whenever you go into placement, set a goal in your mind about what you want to gain out of attending based on the skills required of you as a junior doctor. Ask your supervising clinician which patients would be good to clerk/examine and speak to them about your differential diagnosis as well as coming up with a management plan. Offer to document in the notes during ward rounds (remember to get this countersigned by a doctor), as this will be your bread and butter when you become a Foundation Year 1 doctor. Look up any investigations the patients may have had e.g. blood test results, ABG analysis, ECG, chest x-ray and try to interpret these results yourself before discussing with your doctor. Especially with imaging, it’s not only good practice to interpret what you see but also to present your findings as this could also be asked of you in the OSCE. Seek out opportunities to practise procedures such as cannulation, ABG’s, catheterisation as you are required to be confident in performing these when you become a doctor plus, you get a sign off for your procedures list so it’s a win-win situation.
Geeky Medics is a great resource for learning how to interpret investigations, especially for radiology as they give a clear structure that you can follow. In addition, they have videos and a step by step guide to performing the procedures mentioned above. Another resource I’ve found useful for imaging is Radiology Masterclass.
Make use of your tutors around you
An examination station comes up every year without fail so if you prepare well, these can be easy marks you can obtain on the day. Your twilight tutor sessions (Y4 students) are really good opportunities to practise performing examinations, particularly if you ask to see patients with clinical signs, as you’ll be able to receive personalised feedback and see in person what certain signs look like/sound. Make sure you learn your examinations earlier on, as the closer you get to your exams, the more difficult it can be to balance learning everything in the curriculum so practising this now will be one less thing to worry about later on. In addition to this, after you become confident with the steps of your examination, aim to complete them in timed conditions to replicate the time pressure during the OSCE.
You may also be allocated a tutor for teaching depending on the rotation you’re on, so use these tutorials to go over any topics you find difficult to understand as well as going over skills that you aren’t able to learn from a textbook e.g. prescribing, ward documentation, examination skills or just any of the skills mentioned in the list above. When you get closer to your exams, you might want to do OSCE-Practice style tutorials with your tutor/twilight tutor e.g. I went over paediatric history-taking, ABCDE stations and prescribing with my paediatrics tutor.
Amnesty
Amnesty is a goldmine for practice OSCE stations (mainly for Y5 students) as well as information about stations from previous years. However, be cautious about using these resources as the content has not been checked for accuracy by the medical school and some documents contain information about OSCE stations prior to 2018 which could be outdated/incorrect. Therefore, whilst they are useful, do remember to fact-check the information with updated guidance if you’re going to be using the stations for revision.

For Year 5 students, the updated OSCE pack and MBBS Y5 OSCEs Round up are amazing albeit outdated resources for all things related to the OSCEs. It contains multiple mark schemes for all sorts of stations that could potentially come up depending on the speciality, so I really recommend using this as a resource for practising OSCE stations. Not only that but the first few pages contain very detailed information about the content of OSCE stations prior to 2018 so this would be really good for you to read to understand what could be expected of you in your exam. As cliché as it sounds, common conditions are common and in order to prepare you for encountering these as a doctor, certain topics can be tested repeatedly; however, do be mindful that the content and station focus changes each year. Therefore, when using these resources for revision, be cautious with the information as the curriculum has changed since 2018. These Amnesty mark schemes are more beneficial for revision purposes as opposed to being indicative of what the summative mark scheme will entail so check the sample OSCE stations on the Moodle Assessment & Feedback page for guidance.
With a prescribing task being a feature of many OSCE stations in your summatives, I found running through the different scenarios in the Acute Prescribing presentation (specific to Y5) to be really helpful and would encourage you to do the same. These are just some of the documents I personally used the most when revising for OSCEs, however there’s lots more that you can go through to get more insight into your exam.
Mock OSCE
A mock OSCE is a formative assessment which is designed to simulate your summative OSCE in order for you to get a flavour of how your exam day will run. It’s a brilliant learning experience, as you will have the opportunity to practise various different skills, assess your ability to perform under time pressure and you’ll get feedback which should enable you to plug any gaps in your knowledge. Plus, as this assessment doesn’t count towards anything, it’s the perfect place to make mistakes as that’s how you’ll learn from them.
For those of you in Year 4, you should have a clinical skills mock OSCE at the end of your Module B placement, where you will have stations going through different procedures that you were taught during your clinical skills sessions. Make sure to utilise this session carefully and retain the mark schemes for practice as these procedural skills can be tested. UCL Medical and Surgical Society also organise mock OSCEs, so make sure you like their Facebook pages to keep up to date with any mock OSCE announcements.
For Year 5 students, you will have numerous workshops dotted throughout each module; some of which involve actors and tutors for supervision. These are really useful sessions which test your consultation skills as done in the OSCE.
There’s a lot of information to digest here, but don’t worry you have time and if you pace yourselves from now until the end of the academic year, you’ll be able to cover a lot of ground. Good luck with your revision and all the best for your exams.
Resources:
- Moodle MBBS Assessment OSCE Resources
- Amnesty on Moodle
- Geeky Medics – https://geekymedics.com
- OSCEstop – https://oscestop.com/notes.html
- OSCE Cases with Mark Schemes – https://www.amazon.co.uk/OSCE-Cases-Mark-Schemes-Revision/dp/1848290632
- Clinical Years’ Treasure Trove – https://drive.google.com/drive/folders/1Bf2BH3kiYIV8ogwMFmkLAsu6fFM3ZbLx
- OSCkey – Student teaching from older UCL medics tailored to the clinical skills tested in the OSCE
- OSCE sense (Practice OSCE Stations) – https://www.oscesense.com
 I enjoy writing helpful tips about how to make the most of your time at medical school. Being from Liverpool, London seemed intimidating and intense at first, but I’v
I enjoy writing helpful tips about how to make the most of your time at medical school. Being from Liverpool, London seemed intimidating and intense at first, but I’v
 I can’t quite believe I’m reaching the end of medical school, but I’m excited to share the experiences I’ve had along the way and tips I wish I knew to make the most of your time here. Despite being a Londoner for most of my life (I was born in Norway), I enjoy trying out new food places and playing badminton in my spare time.
I can’t quite believe I’m reaching the end of medical school, but I’m excited to share the experiences I’ve had along the way and tips I wish I knew to make the most of your time here. Despite being a Londoner for most of my life (I was born in Norway), I enjoy trying out new food places and playing badminton in my spare time. Despite having lived in five different parts of the world already, the last five years have still been a fresh and exciting mixture of ups and downs as I tried adapting (still am adapting in all honesty) to the university lifestyle. I’m excited to share some of my experiences with you in this guide and hopefully give you a few tips along the way. Outside of medicine I enjoy travelling, films, and most things coastal-side. Feel free to email any questions, concerns, or if you just want to have a chat.
Despite having lived in five different parts of the world already, the last five years have still been a fresh and exciting mixture of ups and downs as I tried adapting (still am adapting in all honesty) to the university lifestyle. I’m excited to share some of my experiences with you in this guide and hopefully give you a few tips along the way. Outside of medicine I enjoy travelling, films, and most things coastal-side. Feel free to email any questions, concerns, or if you just want to have a chat.