Authors: Natalie Bishop1, Hamish Robertson2, Naomi Jones2, Aamina Mahmood1, Lema Delara1, Yasmin Baki2, Camilla Sen2
1UCL Medical School, UCL 2 University College London Hospital, NHS
Introduction
Effective communication within paediatrics is essential to delivering safe, compassionate and professional care. Medical students report a lack of training in this domain. Literature demonstrates that peer role-play is an effective method to teach paediatric communication skills. [1]
We identified a need for more paediatric communication skills teaching, with Equality, Diversity and Inclusion (EDI) integrated throughout, in order to equip future paediatricians to meet the needs of children, young people and families.
Our objective was to co-create a role-play based paediatric communication course for medical students, with an EDI focus. Collaboration between clinicians and students was used to integrate the expertise of paediatric registrars with student perspectives, to ensure outcomes were mapped closely to aims of our university curriculum.
Methods
Our team of undergraduates and paediatric registrars co-created a series of peer role-play scenarios, mark schemes and discussion points.
Themes of protected characteristics were integrated throughout. These were delivered as a communication course for medical students on their paediatric teaching block in their penultimate year of study.
The course was delivered as a pilot of four 90-minute sessions from December 2022 to January 2023 to ten students, with more student groups in the future. Sessions began with introduction to theory, followed by peer role-play and concluded with facilitated discussion and reflection.
Pre- and post-course questionnaires were completed, with feedback used to adapt delivery of the course for future cohorts.
Workflow
Examples of scenarios and EDI elements:
- Performing a HEADSSS assessment on a teenager who is a young carer
- Explaining the need for a child to receive a blood transfusion to parents who are Jehovah’s Witnesses
- Give safety-netting advice to a parent for their child who has diarrhoea and vomiting and lives in a crowded home
An example of the student instructions for one of our scenarios:
Results
Self-reported confidence in paediatric communication increased from 4.9 to 7.3, where 10 is the most confident. 100% of students reported the course was useful and found the scenarios realistic and relevant. Students appreciated the co-creation aspect as their peers are “likely to understand what [they] need”.
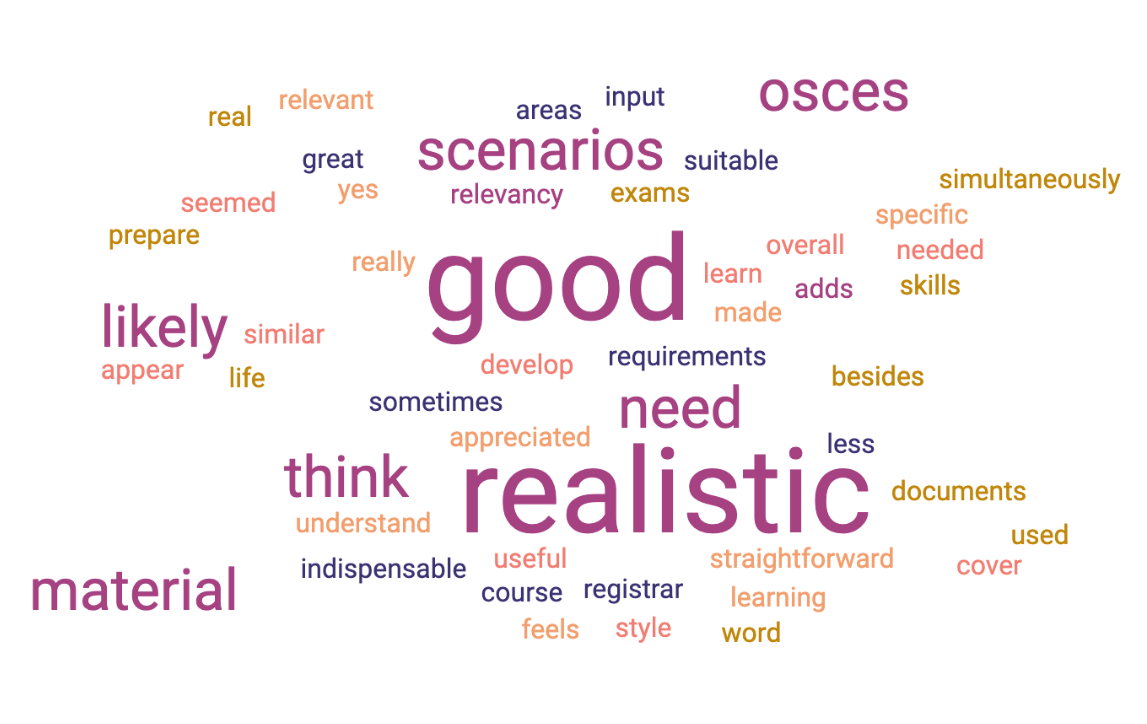
The word cloud below was generated from the qualitative data generated from the question “What do you think about learning from material developed with students?“:
Conclusion
Co-creation between students and doctors enables effective training of undergraduates in paediatric communication skills. It facilitates holistic teaching by integrating students’ perspectives with paediatricians’ clinical expertise.
References
- Frost KA, Metcalf EP, Brooks R, Kinnersley P, Greenwood SR, Powell CV. Teaching pediatric communication skills to medical students. Adv Med Educ Prac. 2015 Jan 16;6:35-43. doi: 10.2147/AMEP.S68413.