Abstract
COVID-19 highlighted the weaknesses in the Medical School Personal Tutor (PT) programme and was the catalyst for its change. Medical students were faced with the challenges of virtual learning, national lockdown, and volunteering to support the national effort in hospitals and the community. Our students needed engaged and supportive PTs; however, there were mixed experiences. After raising this in our student-staff consultative committee (SSCC) meetings, we undertook a collaborative UCL Changemaker project to gain insight into the tutor-tutee relationship.
This helped us develop new resources and implement better tutor training and introductory sessions for students. As we entered the new ‘normal’, we recognised that students’ support needs would be different. We subsequently undertook a larger study focusing on what post COVID-19 learners wanted from their PT and if feasible improvements could be implemented. These study findings have helped us reimagine the PT programme from clarifying its purpose to altering its delivery.
Introduction
COVID-19 was well-recognised as an additional stressor for university students nationally and within our institution (1). Students had to quickly adapt to online and virtual learning methods while facing fears pertaining to the virus and lockdown restrictions. Many also undertook caring responsibilities for family and friends. Medical students were additionally confronted with the demands on the National Health Service (NHS), with many helping whilst on placement, volunteering in intensive care units, and later assisting as vaccinators (2). This was a period where students especially turned to support services for help and needed engaged and supportive Personal Tutors (PTs). There were however mixed experiences of the medical school PT programme reported, with some students regularly meeting with their tutor but a significant number having never met with their personal tutor at all.
The Student Evaluation Questionnaire (SEQ) feedback highlighted these student concerns, which also contributed to a feeling of dissociation from the Medical School. Many students were not meeting with their personal tutor, and a concern about the paucity of support was raised in our Student-Staff Consultative Committee (SSCC) meetings. As a high priority, we therefore undertook a student-led UCL Changemaker project to find out more about student and tutor experiences of the existing PT programme and review the dynamics of the tutor-tutee relationship. Following on from this, a further study was conducted to identify what students needed from the personal tutor programme.
Together, our research has helped us reimagine the PT programme: from clarifying its purpose, to altering its delivery. Herein, we will outline our pertinent results, linking them to our outcomes.
Methods

Our UCL Changemaker project was a mixed methods study conducted in early 2021. Initially, we centred our research on Year 3 students, as they were felt to be in the best position to reflect on the PT programme and share any useful observations, half-way through their MBBS course and after having experienced personal tutoring from a different department during their iBSc.
We initially reflected on informal feedback from discussions with both students and staff, via the Student Evaluation Questionnaire and comments within the SSCC. This helped inform our Opinio survey, which was completed by 39/302 (12.9%) students. Next, we held our first focus group with 4 students (Focus Group 1) to discuss key points raised in the survey and gain a more thorough understanding of student experiences. We then used our survey and Focus Group 1 findings to create preliminary resources. These resources were subsequently evaluated in our second focus group with the 4 students (Focus Group 2) alongside an additional focus group with 5 PTs (Focus Group 3).
Involving PTs enabled us to understand their perspective and their difficulties in establishing successful relationships with their tutees. To acknowledge their contributions, all focus group participants received a £10 gift voucher. Once data collection was completed, we undertook thematic analysis following Braun and Clarke’s 6 phases (3).
After having completed the UCL Changemaker project, we then undertook a larger evaluation of the UCLMS PT Programme in August 2022. This study was open to all students across Years 1-6 of the programme and therefore allowed us to better assess student experience. It further enabled us to identify if there were varying support needs across different year groups that would require a more tailored approach. Through this additional survey, we intended to identify any further gaps in the support provided as well as explore the impact of the changes we implemented in the interim. In total, 23 students completed part of the survey, and 15 completed the full survey.
Our results were then reflected upon and discussed amongst the Senior Leadership Team to inform changes.
Results
Some of the challenges relating to our existing PT programme were highlighted by students. These included poor responsiveness from PTs, the location and environment of the meetings, and students not feeling comfortable discussing their worries and concerns with a busy clinician. It also reaffirmed the concern that students had a very varied experience with personal tutoring.
From the outset, it became clear that many students had few interactions with their PT, with most only meeting their PT once or twice a year. There were a significant number of students who highlighted that they had never met with their PT, and most suggested that this was partly due to poor responsiveness from PTs, with many students reporting that emails were not replied to.
Our results suggested that the initial meeting between the PT and student was highly influential in determining whether students engaged further with the PT programme or felt comfortable reaching-out to their PT during the year. The nature of the first meeting being a group meeting was overall felt to be beneficial, as students felt there was less pressure. However, they felt all future meetings should be held one-on-one to help facilitate open and honest discussion, especially with regards to pastoral progress.
The logistics and environment in which meetings were held were also commented on. As many PTs are clinicians, there were examples of students meeting their tutors in these settings, but this caused a shift in the dynamics of the relationship. Students “felt [meetings were] like a GP appointment” (Focus Group 1). Likewise, meeting in hospital made students feel inferior and stunted the conversation as they felt their concerns were not sufficiently important to discuss in a busy environment. When asked if students preferred online/virtual meetings, 8/15 (53.3%) preferred in-person meetings, although 6/15 (40.0%) were in-different and 1/15 (6.67%) preferred an online format (Survey 2). Students have noted the convenience of online meetings: “easier to organise and arrange, to fit into both participants’ busy schedules” (Survey 1).
This leads onto another key finding regarding expectations of the PT programme. Both students and PTs felt it was important to further clarify what the PT programme should entail to reduce variability in student experience. A tutor felt “a very clear structure needs to happen between the university and the tutors and the university and the students that is identical so that there isn’t any miscommunication” (Focus Group 3). Similarly, students requested clearer training for tutors to ensure more uniformity. There were, however, some unrealistic requests from students for example, allocating tutors to students by similar interests and expecting tutors to assist students with research opportunities and work experience.
We also identified that students had varying beliefs about the role of a PT and, more broadly, what support the PT programme provides within the context of other UCL support services. Students found that meetings were predominantly academic focused and reported that tutors could be uncomfortable discussing pastoral matters,
“[the tutor was] more concerned with just trying to keep it to school and concerned with grades, instead of actually caring about my, I guess personal life” (Focus Group 1).”
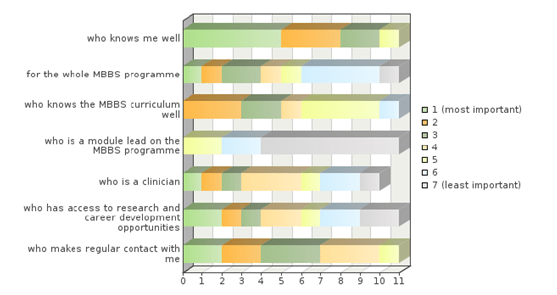
When we asked students what aspects of the PT programme were most important to them, the most popular response was a PT ‘who knows [them] well’ (Survey 2), and most students did value having a PT.
The new resources we created were found to be very positive by the participants in Focus Groups 2 and 3. They particularly found the timelines we created useful; these highlight key milestones during the year and recommend points of discussion for each meeting. We also set out clear tutor and tutee expectations and explained the purpose of the PT programme more in depth. The resources additionally refer to wider support services, which students found “useful just to like have the information in one place” (Focus Group 2). Unfortunately, 9/23 students reported they were not aware of any resources regarding the PT programme including wider university websites and information leaflets (Survey 2), suggesting more could be done to increase their accessibility.
Outcomes
Addressing the poor contact between tutor and tutee, we now ask all PTs to initiate contact with their tutees and recommend three meetings per year (1 meeting per term). Engagement is more closely monitored by the Medical School through online appointment notes. We further encourage students and tutors to maintain contact throughout the year via email to help foster familiarity and for both students and tutors to contact the Personal Tutor team, should there be a lack of engagement from either party.
With regards to the meeting environment, we advise that all first meetings should be held in person in neutral settings. We do see the benefit of having a group meeting initially with the addition of an individual chat one-on-one afterwards to help build rapport. For future meetings, the format can be online/virtual if both individuals are comfortable with this.
To help establish clear expectations, we have now included this in our tutor training and introductory orientation module (IOM) lectures. The tutor training has also been reviewed to now include more information on pastoral support. We also regularly update tutors on changes to support services within the Medical School and wider university policy, as we recognised that a barrier to tutors providing pastoral support was poor information and communication. A monthly online seminar series has been introduced, to help further develop the skills of our Personal Tutors. For the early year tutors (Years 1-2) we have also moved to employing dedicated PTs who have time within their job plans and are more well supported by the Senior Leadership Team.
In the IOM lectures, to improve student engagement, we further emphasise the purpose of the PT programme and ensure to explain the role of a PT, highlighting relevant wider support services as well. We have also signposted our new resources and circulate them via email and course pages regularly. To further improve the PT programme, we continue to collate both informal and formal feedback from students to help implement improvements.
Conclusion
An engaged PT can have a significant benefit to the student in terms of academic and pastoral support (4). Through a staff, student collaborative project, we were able to identify student expectations and needs with regards to our PT programme at the medical school and implement improvements.
Our PT programme remains under constant review, and more recently, we have moved to a system of having fewer, better trained tutors for a larger number of students and will continue to evaluate this adjustment.
References
- Campbell F, Blank L, Cantrell A, Baxter S, Blackmore C, Dixon J, et al. Factors that influence mental health of university and college students in the UK: a systematic review. BMC Public Health [Internet]. 2022; 22(1):[1778 p.]. Available from: DOI: 10.1186/s12889-022-13943-x.
- UCL. Supporting COVID effort 2024 [cited 16th March 2024]. Available from: https://www.ucl.ac.uk/medical-sciences/student-experience/supporting-covid-effort.
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology [Internet]. 2006; 3(2):[77-101 pp.]. Available from: DOI: 10.1191/1478088706qp063oa.
- Woods A, Lefever R. Case Study 23. Student Success Coaching: developing a model to enhance personal tutoring and student success. In: Walker B, Stork A, Lochtie D, editors. The Higher Education Personal Tutor’s and Advisor’s Companion: Translating theory into practice to improve student success. St Albans: Critical Publishing; 2022. p. 155-161.