Author: Katie E. Wardle
Co-authors: Ellie Nash, Emma Kelley and Sarah Bennett
Abstract
During the COVID-19 pandemic, the “clinical apprenticeship” model was introduced at UCLMS to aid learning; students were encouraged to participate in daily clinical activities and staff were provided with guidance on apprenticeship-style teaching. Student feedback of the model’s efficacy varied, prompting a mixed-methods research study to evaluate the apprenticeship model from the student perspective. Data from a Years 4-6 survey (n=45) and Year 5 student focus group (n=5) were thematically analysed to identify initial key themes: Poor clinical staff awareness of the apprenticeship model; Feeling part of the team; The importance of feeling valued and being given responsibilities; The value of observational learning depends on experience; Poor student understanding of expectations from the apprenticeship model. Once we have completed and analysed pending focus groups, all results will be shared with staff to feed into making future improvements to the clinical apprenticeship model to provide a more fulfilling student experience.

Introduction
- Clinical placements form an essential part of academic success in medical school; students develop core skills through completing mandatory course requirements to prepare them for assessments and their future career.
- The COVID-19 pandemic transformed the clinical learning environment (Papapanou, 2021; Triemstra, 2021). With the reinstatement of clinical placements, which had been cancelled during the peak of the pandemic, it was well recognised that students would require guidance on how to make the most out of their learning opportunities in a busy workplace (GMC 2021).
- The “clinical apprenticeship” model was introduced at UCL Medical School (UCLMS) to aid learning for students on clinical placements which included Year 4, 5 and 6 students.
- This model aimed to encourage students to immerse themselves in the day-to-day activities of a busy clinical environment with staff provided with guidance on apprenticeship-styles of teaching.
- However, comments and anecdotal reports suggested that students feared that their learning had been compromised; gaining formalised feedback on this model was therefore crucial.
- A mixed-methods research study was conducted with the aim of evaluating the apprenticeship model from the student and staff perspective using a survey and focus groups. Feedback will be utilised to improve the student experience and associated academic success.
Methods
- The first stage of our project involved evaluating the clinical apprenticeship model from the student perspective through a survey and focus groups.
- This project received ethical approval from UCL Ethics Committee and follows BERA ethical guidelines.
- The quantitative data from the survey was analysed to provide an indication of the perceived success of the apprenticeship model.
- The qualitative data from both the survey and focus groups will be thematically analysed to identify key themes.
Survey
- Year 4-6 medical students were invited to participate voluntarily in a survey consisting of 22 questions, including Likert scales and free-text answer options.
Focus groups
- Years 4-6 students were invited to participate in a focus group. We plan to hold one focus group per year group.
- Each focus group will be led by one trained researcher who will follow a script and set of questions to standardise the focus groups and limit bias.
- Focus groups will be conducted online using Microsoft Teams, recorded and transcribed verbatim by the researchers.
Initial Results
- Currently, we have successfully conducted the Year 5 focus group and are awaiting scheduling the Year 4 and 6 focus groups.
- 45 surveys were completed across the three year groups:
| Year group | Number of surveys completed |
| Year 4 | 9 |
| Year 5 | 18 |
| Year 6 | 19 |
- Students submitting the survey were based at one of the following clinical sites: University College Hospital, The Royal Free – Barnet Hospital, Whittington Hospital, District General Hospitals and GP practices (Year 6 only).
- Students were asked “What does the “apprenticeship model” mean to you?” Learning through “active participation” and as “part of a team” featured frequently.

Key quantitative findings
- 86% were aware that the apprenticeship model had been implemented.
- 84% felt that their confidence in communicating effectively with patients and relatives had developed.
- 78% felt that they had developed their clinical skills.
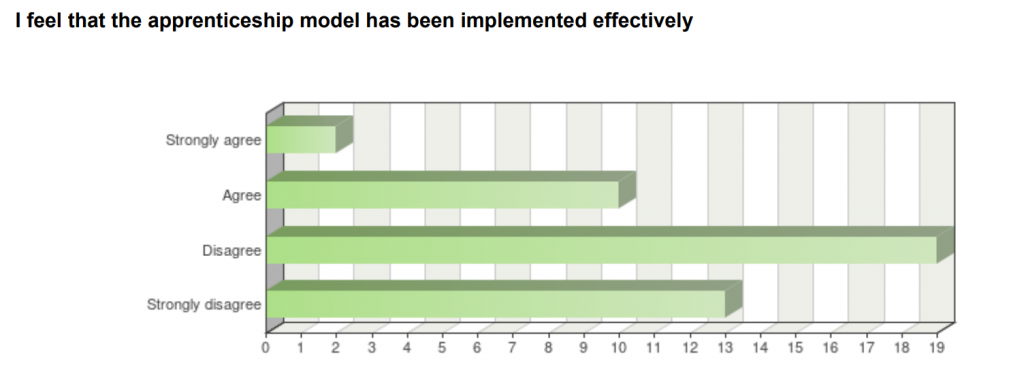
- The majority of respondents disagreed or strongly disagreed with the statement “I feel that the apprenticeship model has been implemented effectively” (n=32).
- Most respondents also disagreed/strongly disagreed with the statement “The clinical staff at the hospital sites understood the apprenticeship model” (n=32).
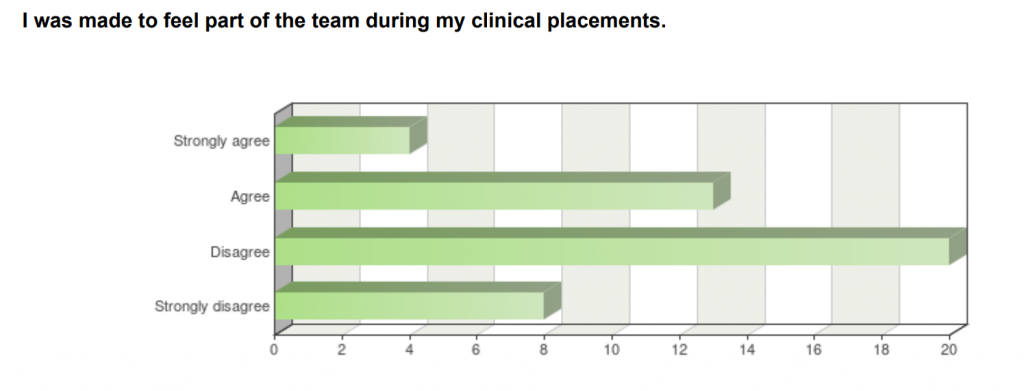
- “I was made to feel part of the team during my clinical placements” was a further statement which most respondents disagreed or strongly disagreed with (n=28).
- Students were asked about the frequency they had been given opportunities to participate in different clinical tasks. This table compares the clinical tasks which the majority of students had frequent (at least fortnightly) opportunities to complete compared to those which students had never had the opportunity to complete.
| The majority of students had opportunities to complete these clinical tasks at least fortnightly | The majority of students had never had the opportunity to complete these clinical tasks |
| Attend an outpatient clinic | Write discharge summaries |
| Attend a handover meeting | Involved in transferring stable patients |
| Observe a procedure/surgery | Assist with patient care (e.g. feeding) |
| History gathering | Shadowing a drug round |
| Physical examination | Attend a medical emergency/cardiac arrest |
Key themes
Researchers agreed upon initial key themes from the qualitative data in the survey free-text answers and the Year 5 focus group:
Poor clinical staff awareness of the apprenticeship model
- Students felt that clinical staff were unaware of the model and lacked knowledge of students capabilities.
“..we’ve had a registrar or consultants who are very kind of hands off, they don’t want us coming near them, ask anything, or say anything”.
“we WANT to be involved, we don’t like standing around watching or doing nothing or not being spoken to/asked questions. it’s really frustrating”.
Feeling part of the team
- Feeling part of the team was highlighted as being extremely important to students.
- Many students who reflected on positive experiences of the apprenticeship model explained how they were made to feel part of the team and felt welcomed by staff.
“Anaesthetics rotation – team were really warm, were keen to teach students and get them involved in every aspect of the anaesthesia”.
“I feel like I’m more of a burden to the team rather than I’m actually part of the team.”
The importance of feeling valued and being given responsibilities
- Year 5 and 6 students reflected on positive experiences where they were made to feel a valuable team member and given responsibilities.
“..the times that the apprenticeship model has worked well… when I’m either seeing the patient myself and I need to get some data, some information I mean to feed that back to my senior, and we need that for the plan, because there’s really an onus on me to actually do something.”
“There’s a reason why I’m there and… I’m useful to the team”.

The value of observational learning depends on experience
- Students commented that learning only through observation was not enough and they learned better when they actively participated in clinical activities. This was highlighted particularly by Year 5 and 6 students.
- Students felt that observing was appropriate when they lacked experience and early on in a placement but that this should evolve into active learning opportunities.
“I don’t find it that useful to learn through observation, it’s just passive.. I think after the first couple where you do nothing, you just zone out and you very much are just a fly in the wall.”
Poor student understanding of expectations from the apprenticeship model
- Students felt that learning was “opportunistic” and “situational” with varying experiences across placements and sites.
- Students requested more structured teaching opportunities and clear learning expectations from each placement.
“Part of the apprenticeship model was very welcoming and everyone, from FY1s to consultants got me involved. However in different placements it has been difficult to get the same experience”
“Sometimes I’m just a fly on the wall and then I’m not doing anything”.
Future Planning
- We will shortly be conducting the Year 4 and 6 focus groups. Results from this will feed into our preliminary thematic analysis.
- We are also conducting an anonymous online survey to gain feedback from the clinicians delivering the clinical apprenticeship model.
- The results will be shared with the relevant staff to discuss future improvements to the clinical apprenticeship model for the next academic year.
- We hope that these changes will provide a more fulfilling student experience which feeds into academic success.
- We hope to publish this data to share current knowledge and key learning regarding using the clinical apprenticeship learning in medical education.
Authors and Contributors
Dr Katie Wardle, Dr Ellie Nash, Dr Emma Kelley and Dr Sarah Bennett
Acknowledgements
We would like to thank all of the students that participated in our survey and focus group.
References
General Medical Council (GMC) (2021). https://www.gmc-uk.org/news/coronavirus/coronavirus-information-for-medical-students Published March 2021. (Accessed online 28.6.21)
Papapanou M, Routsi E, Tsamakis K, et al. (2021). Medical education challenges and innovations during COVID-19 pandemic. Postgraduate Medical Journal Published Online. doi: 10.1136/postgradmedj-2021-140032
Triemstra JD, Haas MRC, Bhavsar-Burke I, et al. (2021). Impact of the COVID-19 Pandemic on the Clinical Learning Environment: Addressing Identified Gaps and Seizing Opportunities. Academic Medicine : Journal of the Association of American Medical Colleges. Sep;96(9):1276-1281.