Author: Dr. Sara Al-Khafaji
Background
The appearance of the unprecedented Coronavirus Disease 2019 pandemic (COVID-19) (Darras et al., 2021) has created a sudden and noticeable shift towards the exclusive usage of online learning environment as the main source of medical education (Dost et al., 2020).
Delivering CBL virtually to medical students is an exciting educational prospect. Although there is a plethora of literature on CBL within medical education, there is a paucity of literature within the contexts of electronic CBL(e-CBL), where the literature seems to be scant and unfocused. Therefore, the aim of this literature review is to evaluate the role and significance of e-CBL within medication education. This will be used to inform medical schools of the value of using e-CBL to teach 21st century medical students.
Methods
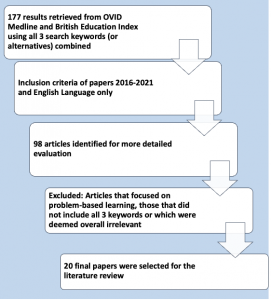
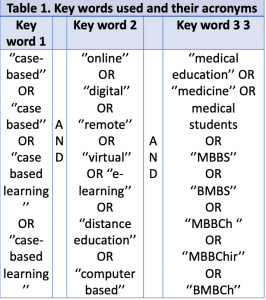
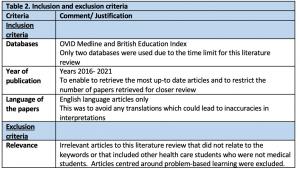
OVID Medline and British Education Index databases were searched with a keyword search strategy (Table 1) which was utilised to limit searches to literature within the topic area. Each key word searched included alternatives to allow for their respective acronyms. Inclusion and exclusion criteria were used as shown below (Table 2).
Results
-
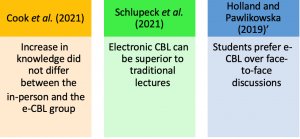
Comparison with face-to-face CBL
Interestingly, Cook et al. (2021) found the increase in knowledge did not differ between the in-person and the e-CBL group. This is however, in contrast, to the results by Schlupeck et al. (2021) which suggests that e-CBL can be superior to traditional lectures when it comes to assessing wound care. This is further echoed by the findings of Holland and Pawlikowska (2019)’ study, which found that students prefer e-CBL over face-to-face discussions. However they do surprisingly note that more students(nearly twice) participated in the in-person discussions than completed the e-CBL, making such conclusions contradictory and questioning the overall superiority of an online environment as compared to a traditional face-to face- one.
Overall, there is still considerable uncertainty with how e-CBL compares to an- in person approach due to the lack of literature that discusses this. The majority of the papers which evaluate e-CBL also fail to attempt to directly compare it with a face-to face teaching.
-
Improving test scores
Recently published papers Elsayes et al. (2021), Cook et. al (2021) and Grover et. al (2020), assessed the effectiveness of delivering e-CBL to medical students using ‘’pre-session’’ and ‘’post-session’’ multiple-choice questions (MCQ) to evaluate for an increase in students’ knowledge. All three papers gathered data in a similar method (MCQs) and found a marked improvement of the test scores of medical students after delivering e-CBL sessions.
-
Beyond MCQ scores
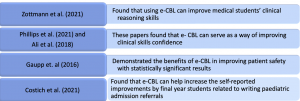
As the COVID-19 pandemic required the medical education systems to advance into a new era of digital learning over a short period of time (Fatani, 2020), unsurprisingly, most of the literature that evaluate the effectiveness of e-CBL is based on short studies and short trial modules. Below are some of the key studies and their findings.
Conclusions and moving forward
Overall, the delivery of e-CBL to medical students has generally shown to be effective way of facilitating learning, improving learning outcomes and increasing knowledge of medical students across different specialties. There is also a satisfactory agreement between papers that students find e-CBL to be an enjoyable and flexible way of learning, which is encouraging in emergency situations such as the COVID-19 pandemic that took place, where e-learning may be the only option. Other key themes discussed in the literature review centred on the advantages and disadvantages of e-CBL and how it compares with other types of learning.
Further research is however necessary to assess the long-term benefits of using e-CBL looking to assess whether the increased knowledge retains over time. Additionally, the findings regarding the superiority of e-CBL when compared directly to other types of teaching, such as face-to-face teaching still remains unclear and require further experimental research.
Dr. Al-Khafaji
MBBS (Hons)
Post graduate Medical Education student (UCL)
Link to the paper’s poster
poster for conference
Bibliography
- Cook, J., Puckett, H. L. and Steinauer, J. E. (2021) ‘Management of Obesity During Pregnancy and Periconception: Case-Based Learning for OB/GYN Clerkships’, MedEdPORTAL : the journal of teaching and learning resources, 17, p. 11129. doi: 10.15766/MEP_2374-8265.11129.
- Costich, M. et al. (2021) ‘Transition-to-residency: pilot innovative, online case-based curriculum for medical students preparing for pediatric internships’, Medical Education Online, 26(1). doi: 10.1080/10872981.2021.1892569.
- Darras, K. E. et al. (2021) ‘Undergraduate Radiology Education During the COVID-19 Pandemic: A Review of Teaching and Learning Strategies’, Canadian Association of Radiologists Journal, 72(2), pp. 194–200. doi: 10.1177/0846537120944821.
- Dawson, J. Q., Ching, G. and Huynh, H. (2021) ‘Lessons in implementing virtual case-based learning’, Medical Education, 55(5), p. 662. doi: 10.1111/MEDU.14515.
- Dost, S. et al. (2020) ‘Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students’, BMJ Open, 10(11), p. e042378. doi: 10.1136/BMJOPEN-2020-042378.
- Elsayes, K. M. et al. (2021) ‘Multidisciplinary Approach in Teaching Diagnostic Radiology to Medical Students: The Development, Implementation, and Evaluation of a Virtual Educational Model’, Journal of the American College of Radiology, 18(8), pp. 1179–1187. doi: 10.1016/J.JACR.2021.03.028.
- Fatani, T. H. (2020) ‘Student satisfaction with videoconferencing teaching quality during the COVID-19 pandemic’, BMC Medical Education, 20(1). doi: 10.1186/S12909-020-02310-2.
- Gaupp, R., Körner, M. and Fabry, G. (2016) ‘Effects of a case-based interactive e-learning course on knowledge and attitudes about patient safety: A quasi-experimental study with third-year medical students’, BMC Medical Education, 16(1). doi: 10.1186/S12909-016-0691-4.
- Grover, S., Garg, B. and Sood, N. (2020) ‘Introduction of case-based learning aided by WhatsApp messenger in pathology teaching for medical students’, Journal of Postgraduate Medicine, 66(1), pp. 17–22. doi: 10.4103/JPGM.JPGM_2_19.
- Holland, J. C. and Pawlikowska, T. (2019) ‘Undergraduate Medical Students’ Usage and Perceptions of Anatomical Case-Based Learning: Comparison of Facilitated Small Group Discussions and eLearning Resources’, Anatomical Sciences Education, 12(3), pp. 245–256. doi: 10.1002/ASE.1824.
- Jurjus, R. A. et al. (2016) ‘Curricular response to increase recall and transfer of anatomical knowledge into the obstetrics/gynecology clerkship’, Anatomical sciences education, 9(4), pp. 337–343. doi: 10.1002/ASE.1587.
- Lim-Dunham, J. E. et al. (2016) ‘A Vertically Integrated Online Radiology Curriculum Developed as a Cognitive Apprenticeship: Impact on Student Performance and Learning’, Academic Radiology, 23(2), pp. 252–261. doi: 10.1016/J.ACRA.2015.09.018.
- Lorenzo-Alvarez, R., Pavia-Molina, J. and Sendra-Portero, F. (2018) ‘Exploring the Potential of Undergraduate Radiology Education in the Virtual World Second Life with First-cycle and Second-cycle Medical Students’, Academic Radiology, 25(8), pp. 1087–1096. doi: 10.1016/J.ACRA.2018.02.026.
- Mukhopadhyay, S. et al. (2021) ‘Evolution of pathology teaching for MBBS students during COVID-19 pandemic lockdown: Moving from a real to a virtual classroom’, Indian Journal of Pathology and Microbiology, 64(3), pp. 524–527. doi: 10.4103/IJPM.IJPM_665_20.
- O’Doherty, D. et al. (2018) ‘Barriers and solutions to online learning in medical education – an integrative review’, BMC Medical Education 2018 18:1, 18(1), pp. 1–11. doi: 10.1186/S12909-018-1240-0.
- Pasarica, M. and Kay, D. (2020) ‘Teaching lifestyle medicine competencies in undergraduate medical education: Active collaborative intervention for students at multiple locations’, Advances in Physiology Education, 44(3), pp. 488–495. doi: 10.1152/ADVAN.00148.2019.
- Phillips, A. L. et al. (2021) ‘Slack as a virtual undergraduate dermatology community: a pilot study’, Clinical and Experimental Dermatology, 46(6), pp. 1028–1037. doi: 10.1111/CED.14601.
- Roth, C. G. et al. (2020) ‘Teaching laboratory stewardship in the medical student core clerkships pathology-teaches’, Archives of Pathology and Laboratory Medicine, 144(7), pp. 883–887. doi: 10.5858/ARPA.2019-0329-OA.
- Thistlethwaite, J. E. et al. (2012) ‘The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23’, https://doi.org/10.3109/0142159X.2012.680939, 34(6). doi: 10.3109/0142159X.2012.680939.
- Wadowski, P. P. et al. (2019) ‘Case-based blended eLearning scenarios—adequate for competence development or more?’, Neuropsychiatrie, 33(4), pp. 207–211. doi: 10.1007/S40211-019-00322-Z.
- Zhao, W. et al. (2020) ‘The effectiveness of the combined problem-based learning (PBL) and case-based learning (CBL) teaching method in the clinical practical teaching of thyroid disease’, BMC Medical Education 2020 20:1, 20(1), pp. 1–10. doi: 10.1186/S12909-020-02306-Y.